What is a sleeve Gastrectomy?
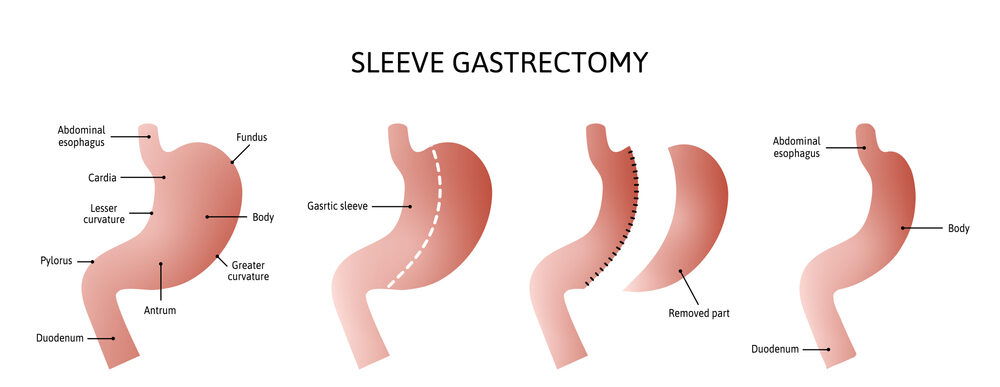
Sleeve gastrectomy or vertical sleeve gastrectomy is a weight-loss surgical procedure. The surgery is performed laparoscopically, by inserting small instruments through small incisions in the upper abdomen. about 80% of the stomach is removed during the sleeve gastrectomy, a, to become tube-shaped like how the picture shows it.
Reducing your stomach restricts how much food you are able to consume. In addition, the procedure prompts hormonal changes that assist with weight loss. These same hormonal changes also help relieve conditions associated with being overweight, such as high blood pressure or heart disease
Sleeve gastrectomy is also different from gastric banding (also called gastroplasty), which consists of placing an adjustable band (gastric band with adjustable diameter), around the upper part of the stomach of patients. The procedure slows down the passage of food, without disturbing digestion.
Why make a sleeve?
Making a sleeve is necessary in case of severe obesity. In the case of BMI (Body Mass Index) greater than 40. Or in case of BMI between 35 and 40 with associated complications (high blood pressure, sleep apnea, type 2 diabetes, heart problems, etc.).
The sleeve, by considerably reducing the size of the stomach, will generate a feeling of satiety much more quickly and allow weight loss of around 30 kg on average in the first year following the operation. The risks of this procedure are moderate, and the occurrence of complications is rare.
Who is affected by a sleeve?
To be eligible for the sleeve, the patient suffering from obesity must have exhausted other means of losing weight (diet, physical activity, etc.). And it must meet certain conditions:
- His BMI must be that of morbidly obese, i.e. greater than or equal to 40.
- The patient must be between 18 and 60 years old. This procedure is not performed on children.
- The patient must not have any medical contraindications to this bariatric surgery (hiatal hernia, gastroesophageal reflux, heavy history of abdominal surgery, etc.) or any psychological contraindication.
How to prepare for a sleeve?
All sleeves are subject to a preoperative follow-up of 6 to 12 months. This follow-up is essential to the success of the sleeve. A multidisciplinary team made up of a gastroenterologist, an anesthetist, a surgeon, a psychologist, a dietician, a nutritionist, a physiotherapist, and a pulmonologist will define a program for the patient, with monthly adjustments.
This will consist in particular in making the patient adopt a new lifestyle that involves taking balanced meals, as well as the daily practice of physical activity compatible with his weight.
How is a sleeve performed?
The sleeve gastrectomy operation is a surgical procedure performed under general anesthesia. In the absence of complications, this operation lasts between 1h30 and 2h. The operation is performed under laparoscopy and consists of cutting the stomach vertically, suturing the remaining part of the stomach with staples, and extracting the cut part from the abdomen. Hospitalization lasts two days in principle but can be extended to 8 days for more complicated cases. A work stoppage of two weeks is necessary on average.
What are the consequences of a sleeve?
After the operation, a sleeve will require lifelong medical follow-up. Immediately after the intervention, the operated patient will resume a progressive diet, with very reduced rations. For the first 2 or 3 days, only liquid food will be offered. Then he can eat purées, compotes, mixed foods, and finally find a normal diet in its variety but reduced in its quantity. He is therefore supervised by a dietitian. Psychological follow-up is also offered.
Here are, more specifically, the food recommendations of the High Authority for Health:
- Ingest, chewing slowly, small amounts at each meal.
- Take your meals seated and preferably in peace.
- From the first digestive tugs and/or as soon as you have reached satiety, stop eating.
- Drink several times between meals, but avoid doing so while eating;
- Eat a balanced and varied diet to increase your chances of weight loss and avoid nutritional deficiencies;
- Adopt a diet offering an adequate intake of protein (dairy products, eggs, meat, fish);
- Avoid carbonated or sugary drinks, sauces, and fried foods, as well as sweets and other fatty foods.
The failure rate of the sleeve is low. The failure generally comes from the patient’s non-compliance with lifestyle instructions: insufficient food hygiene, and lack of regular physical activity.
The sleeve is a bariatric surgery operation that presents relatively little risk of complication or contraindication. But as rare as they are, they do exist:
- Healing can be bad and generate an ulcer. More seriously, poor healing can generate a fistula, which will allow gastric contents to spread into the belly. This rare but serious complication requires further surgery. A TOGD (Oeso-Gastro-Duodenal Transit), in addition to an oeso-gastric fibroscopy , postoperatively and before the resumption of food, makes it possible to detect a possible fistula.
- An infection can develop at the level of the scar.
- Gastroesophageal reflux, that is to say, the passage of acidic gastric juices in the esophagus, or even the throat, can appear.
- Postoperative hemorrhage may be observed and will require a return to the operating room in order to aspirate the blood clots.
- The stomach may expand.
Our Services
Contact Info
-
Phone: +90-530-844-1477
- Whatsapp: +90-530-844-1477
- info@mednificant.com